Redesigning healthcare payment models around well-defined episodes of care can enhance clinical outcomes while lowering costs.
Healthcare delivery in the United States has traditionally been on a fragmented, fee-for-service model that compensates volume over value. This model has helped drive the nation’s unaffordable healthcare expenditure, which hit $4.5 trillion in 2023—close to 18% of GDP. Episodes of care offer an attractive solution by grouping services associated with a particular condition, procedure, or acute event into a single unit for measurement, management, and payment. But what is an episode of care, and how does this system align incentives between payers, providers, and patients?
Let’s take a closer look:
What is an Episode of Care?
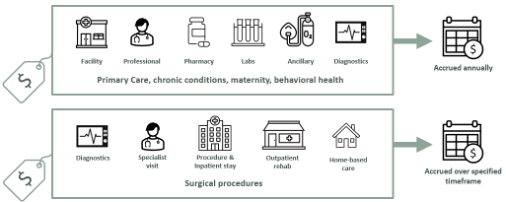
An Episode of Care is a budget-based, time-bound, and clinically anchored way of organizing and paying for healthcare. It includes all services related to the management of a condition or treatment, spanning across providers, care settings, and time. Whether it’s managing a chronic condition or undergoing a surgical procedure, an episode captures the full clinical encounter, not just isolated services.
Episodes offer a more predictable, transparent, and outcome-oriented model of care with increased accountability for cost, quality, and experience across the entire episode. This stands in contrast to traditional fee-for-service models that pay for services individually without regard to coordination, outcomes, or total cost.
Episodes vs. Bundles
While sometimes used interchangeably, Episodes and Bundles are not the same.
- A Bundle typically refers to a predefined group of services delivered over a short timeframe (e.g., imaging, post-op visit, rehab), often tied to a specific procedure or phase of care. It’s limited in scope and may not include all instances of the clinical journey, e.g. a readmission.
- An Episode, in contrast, reflects the entire journey of care for a condition or procedure—from diagnosis and treatment to recovery and follow-up—and includes all relevant services across providers and settings. It is broader, risk-bearing, and intended to reflect the total cost of and accountability for the longitudinal episode.
Episodes create a more retail-like experience for plan members and provide a single, fixed price for comprehensive care.
How do Episodes of Care work?
Operationally, XO Health deploys episodes of care to provide value-based quality and cost improvement. For example, a patient with diabetes (a condition episode) would be attributed to his or her primary care physician or endocrinologist on the basis of claims history or voluntary preference. This physician is now responsible for coordinating all diabetes care throughout the 12-month episode.
At the same time, a patient going through knee replacement surgery (a procedural episode) would have their care attributed to the orthopedic surgeon who is performing the procedure. The episode would encompass a specified lookback period to guarantee proper pre-operative care, the procedure, post-operative rehabilitation, and a warranty period during which the surgeon is still responsible for managing preventable complications.
This structured approach helps eliminate care gaps, reduce unnecessary services, and align incentives toward value-based outcomes rather than service volume, while also ensuring that the most accountable provider is managing each episode.
Episodes of care signify a paradigm change in the way we think about, deliver, and pay for healthcare services. By establishing clear definitions around triggers, attribution, episode timeframes, and measurement methodologies, the XO Health model introduces accountability across the continuum of care while enabling data-driven opportunities for improvement. As healthcare further transitions to value-based payment models, episodes of care offer a framework for measuring and enhancing clinical and financial outcomes.
To find out more about how XO Health applies episodes of care to its value-based care model or to discuss partnership opportunities, contact our team today. Together, we can create a healthcare system that provides better care at lower costs—one episode at a time.